In our continuous quest for better health and well-being, medications often become a central part of our lives, especially for managing chronic conditions. However, while these medications are pivotal in treating various ailments, their long-term use raises important questions regarding their impact on cognitive health.
Cognitive health, a crucial aspect of our overall well-being, encompasses memory, concentration, and the ability to learn and make decisions. Yet, it’s often overlooked in the broader health conversation. As we navigate through the complexities of medications ranging from antidepressants to antihypertensives, understanding their potential effects on our cognitive faculties becomes paramount.
Contents
Types of Medications Often Used Long-Term
In the realm of healthcare, several medications are prescribed for long-term use to manage chronic conditions. These medications, while beneficial for specific health issues, can have varying effects on cognitive health. Here we explore the common types of medications that are often used over extended periods and their potential impact on cognitive functions.
Antidepressants
Antidepressants are widely prescribed for the long-term management of depression and anxiety disorders. They work by altering the balance of neurotransmitters in the brain, which can affect mood and emotional states. Common types of antidepressants include Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), and tricyclic antidepressants. While effective for mood disorders, some studies have raised concerns about their long-term impact on cognitive functions like memory, processing speed, and executive functioning.
Antipsychotics
Antipsychotics are primarily used to treat disorders such as schizophrenia, bipolar disorder, and sometimes for major depressive disorder. These medications target various neurotransmitter systems in the brain, including dopamine and serotonin pathways. Long-term use of antipsychotics, especially the older, first-generation antipsychotics, has been associated with risks such as cognitive dulling, difficulties in concentration, and memory impairments [1].
Antiepileptics
Antiepileptic drugs, also known as anticonvulsants, are used for the long-term treatment of seizure disorders and some types of nerve pain. These drugs can impact the brain’s electrical activity and neurotransmitter levels. Long-term antiepileptic drug use has been linked to cognitive side effects like slowed processing speed, reduced verbal abilities, and memory issues, although the extent varies depending on the specific medication.
Hypnotics and Sedatives
Medications like hypnotics and sedatives, including benzodiazepines and non-benzodiazepine sleep aids, are often prescribed for anxiety and sleep disorders. They work by enhancing the effect of gamma-aminobutyric acid (GABA), a neurotransmitter that induces calmness and relaxation. While effective in the short term, their long-term use can lead to concerns like impaired cognitive function, memory disturbances, and reduced alertness.
Others (e.g., Antihypertensives, Diabetes Medications)
Other medication categories such as antihypertensives (for high blood pressure) and diabetes medications also play a crucial role in long-term disease management. These drugs can have varying effects on cognitive health. For instance, certain antihypertensives have been linked to both protective and detrimental effects on cognition, depending on the medication class and individual patient characteristics. Similarly, diabetes medications, while crucial for controlling blood sugar levels, may have indirect impacts on cognitive health through their effects on metabolic processes [2].

How Medications Affect the Brain and Cognition
The impact of long-term medication use on the brain and cognitive functions is a complex interplay of various biological mechanisms. Different medications can affect the brain in distinct ways, leading to alterations in cognitive abilities.
Neurotransmitter Alterations from Long-Term Medication Use
Many medications used for long-term conditions work by altering neurotransmitter levels in the brain. Neurotransmitters are chemicals that transmit signals across nerve cells and are crucial for proper brain function. For instance, antidepressants often target serotonin or norepinephrine, aiming to correct imbalances associated with depression. While effective for their intended purpose, these alterations can also impact areas of the brain involved in memory, learning, and decision-making. Over time, these changes can lead to noticeable differences in cognitive processes.
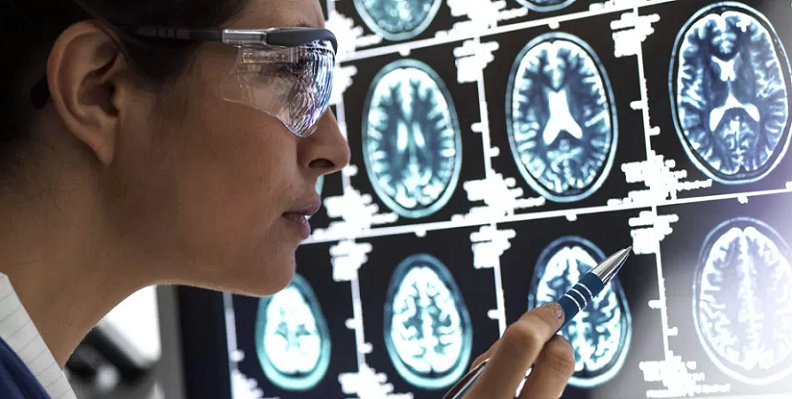
Structural Changes in the Brain Caused by Long-Term Medication Use
Some medications can induce structural changes within the brain over prolonged periods. These changes can include alterations in brain volume, neural connectivity, and the health of brain cells. For example, long-term use of certain antipsychotic medications has been associated with changes in the volume of specific brain regions. These structural modifications can potentially influence cognitive functions like memory formation, spatial navigation, and executive functions [3].
Effects on Memory and Learning Due to Long-Term Medication Use
Memory and learning are fundamental cognitive processes that can be affected by long-term medication use. Drugs such as benzodiazepines, commonly prescribed for anxiety and sleep disorders, are known to impact short-term memory and the ability to form new memories. Similarly, some antiepileptic drugs can affect learning abilities and recall by altering neuronal excitability and synaptic transmission, which are critical for these cognitive functions.
Long-Term Medication Use Impact on Attention and Executive Functions
Attention and executive functions, which include skills like planning, problem-solving, and multitasking, are also vulnerable to the effects of long-term medication use. Medications that induce drowsiness or sedation, such as certain sleep aids and anti-anxiety drugs, can diminish alertness and impair the ability to focus. Moreover, drugs that affect neurotransmitter systems like dopamine and serotonin can influence executive functions, leading to challenges in organizing thoughts, managing time, and making decisions.
Specific Risks Associated with Long-Term Medication Use
While medications are vital for managing various health conditions, their long-term use is not without risks, especially concerning cognitive health. Understanding these risks is crucial for patients and healthcare providers to make informed decisions and manage treatments effectively.
Cognitive Impairment from Long-Term Medication Use
One of the most concerning risks of prolonged medication use is cognitive impairment. This can manifest in various forms, such as reduced memory capacity, diminished concentration, and slower processing speeds. For instance, long-term use of benzodiazepines has been linked to an increased risk of cognitive decline, particularly in older adults. Similarly, chronic use of anticholinergic drugs, which are used in a variety of conditions like allergies and gastrointestinal disorders, has been associated with memory impairment and reduced cognitive flexibility [4].
Risk of Developing Dementia from Long-Term Medication Use
Certain medications, when used over an extended period, may increase the risk of developing dementia. Research has indicated that continuous use of medications with strong anticholinergic properties can lead to an increased risk of dementia, particularly in the elderly. Similarly, long-term use of some benzodiazepines and antipsychotics has also been linked to an elevated risk of dementia. It is important to note that this risk can vary based on the type of medication, dosage, and individual patient factors.
Dependency and Withdrawal Issues Resulting from Long-Term Medication Use
Dependency and withdrawal are significant concerns with certain medications, especially those prescribed for anxiety, sleep disorders, and pain management. Dependence on these medications can lead to a cycle where cognitive functions are further impaired due to the need for continuous medication use. Additionally, withdrawal from these drugs can be challenging and may exacerbate cognitive symptoms, creating a complex situation for patients who need to discontinue or change their medication.
Mitigating the Cognitive Risks of Long-Term Medication
Acknowledging the cognitive risks associated with long-term medication use is vital, but equally important is exploring strategies to mitigate these risks.
Strategies for Safe Medication Management
Safe medication management is key in reducing the cognitive risks associated with long-term drug use. This involves regular review and monitoring of medication regimens by healthcare providers. It’s essential to assess the necessity of each medication, considering factors such as dosage, duration, and potential interactions. Simplifying medication regimens, where possible, can also reduce the risk of adverse cognitive effects. This might include tapering off medications that are no longer necessary or replacing them with alternatives that have a lower risk of cognitive impairment [5].
Role of Regular Monitoring and Assessment When Using Medication Long-Term
Regular monitoring and assessment by healthcare professionals are critical in managing the cognitive risks of long-term medication use. This includes periodic cognitive testing to detect any changes in memory, attention, or other cognitive functions. Additionally, monitoring for physical side effects and interactions between multiple medications is crucial. Patients should also be encouraged to report any cognitive changes they notice, as early detection can lead to more effective management strategies.
Lifestyle Adjustments to Support Cognitive Health
Lifestyle adjustments can play a significant role in supporting cognitive health, particularly for those on long-term medication. Engaging in regular physical exercise, maintaining a balanced diet rich in brain-healthy nutrients, and ensuring adequate sleep are fundamental components. Mental stimulation through activities like reading, puzzles, and learning new skills can also support cognitive function. Additionally, stress-reducing practices such as mindfulness, yoga, or meditation can be beneficial in mitigating the cognitive risks associated with medication use.
Alternative Therapies and Approaches to Long-Term Medication
Exploring alternative therapies and approaches can offer additional support in mitigating cognitive risks. This might include complementary therapies such as acupuncture, herbal supplements, or biofeedback, which some individuals find beneficial. However, it’s important to approach these alternatives cautiously and always discuss them with healthcare providers to ensure they do not interfere with the existing medication regimen.
References
[1] Utilization of Prescription Medications with Cognitive Impairment Side Effects
[2] The Effects of Long-term Medication Use in Alzheimer Disease
[3] Long-term Cognitive and Functional Effects of Potentially Inappropriate Medications
[4] Caution! These Drugs Can Cause Memory Loss
[5] Do prescription opioids impact cognitive function in older adults?