The gut-brain axis has long been a fascinating topic for scientists, revealing the remarkable connection between our digestive system and cognitive health. This complex communication network not only governs how we digest food but also plays a crucial role in our mental well-being. Here we delve into the intricate world of the gut-brain axis and explore how the trillions of microorganisms residing in our gut, collectively known as the microbiome, impact cognitive function.
Contents
Understanding the Gut-Brain Axis
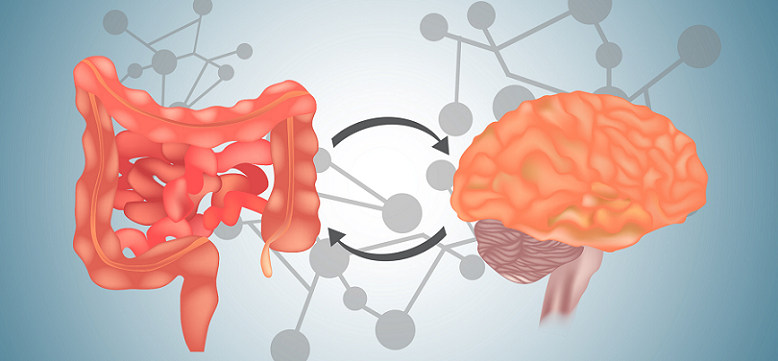
The gut-brain axis is a term used to describe the bidirectional communication network between the central nervous system (CNS), which includes the brain and spinal cord, and the enteric nervous system (ENS), a complex network of neurons embedded within the lining of the gastrointestinal (GI) tract. This intricate connection between the gut and the brain plays a significant role in maintaining our overall health and well-being.
The gut-brain axis encompasses various communication channels, including neural, endocrine, and immune pathways, that allow the gut and brain to exchange information. This constant communication enables the brain to influence gut functions, such as motility and secretion, and allows the gut to relay information about its environment and internal state to the brain.
Role of the Vagus Nerve
The vagus nerve is a key component of the gut-brain axis, serving as the primary neural connection between the gut and the brain [1]. As the longest cranial nerve, it originates in the brainstem and extends to various organs, including the heart, lungs, and GI tract. The vagus nerve carries signals in both directions, transmitting information from the brain to the gut and vice versa. It plays a crucial role in regulating gut motility, secretion, and inflammation, as well as modulating brain functions related to mood, stress, and cognition.
Neurotransmitters and Hormones Involved
Several neurotransmitters and hormones are involved in the gut-brain axis, facilitating communication between the gut and the brain [2]:
- Serotonin: Approximately 90% of the body’s serotonin, a neurotransmitter associated with mood regulation, is produced in the gut. Serotonin plays a vital role in gut motility and is involved in the modulation of mood, appetite, and sleep in the brain.
- Dopamine: This neurotransmitter is involved in reward, motivation, and motor control. While most dopamine is produced in the brain, a small amount is also synthesized in the gut, where it helps regulate gut motility.
- Cortisol: This hormone, released in response to stress, can influence gut function by altering the permeability of the gut barrier and modulating the gut microbiome.
- GABA: Gamma-aminobutyric acid (GABA) is the primary inhibitory neurotransmitter in the brain, and it plays a role in reducing anxiety and promoting relaxation. Certain gut bacteria can produce GABA, which may indirectly influence brain function.
Significance of the Gut-brain Axis in Overall Health
The gut-brain axis is crucial for maintaining overall health, as it influences various physiological processes, such as digestion, immune function, and stress response. An imbalance in the gut-brain axis has been associated with numerous health conditions, including irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), obesity, and mental health disorders like anxiety and depression. By understanding and nurturing this connection, we can potentially improve our physical and mental well-being.
The Gut Microbiome
The gut microbiome refers to the diverse community of microorganisms, including bacteria, viruses, fungi, and other microscopic life forms, that reside in our gastrointestinal tract. These trillions of microorganisms play an essential role in our overall health, impacting digestion, immune function, and even our mood and cognitive abilities.
The gut microbiome is a complex ecosystem that houses various microorganisms that work together to maintain a balanced internal environment. These microorganisms not only help break down the food we consume but also interact with our immune system, produce essential vitamins, and regulate inflammation. The composition of an individual’s gut microbiome is unique, shaped by factors such as genetics, diet, and lifestyle.
Importance of a Diverse and Balanced Microbiome
A diverse and balanced gut microbiome is crucial for overall health, as it helps maintain the integrity of the gut barrier, modulate the immune system, and synthesize important compounds like short-chain fatty acids (SCFAs) and neurotransmitters [3]. A healthy gut microbiome can also protect against pathogenic bacteria by competing for resources and producing antimicrobial substances. Imbalances in the gut microbiome, known as dysbiosis, have been linked to various health conditions, including obesity, type 2 diabetes, inflammatory bowel disease, and mental health disorders.
Factors Affecting the Gut Microbiome
Numerous factors can impact the composition and diversity of the gut microbiome, including:
- Diet: Diet is one of the most influential factors affecting the gut microbiome. The consumption of diverse plant-based foods, rich in fiber, can support the growth of beneficial bacteria, while diets high in saturated fat, sugar, and processed foods can promote the growth of harmful bacteria and contribute to dysbiosis.
- Stress: Chronic stress can negatively impact the gut microbiome by altering its composition, reducing bacterial diversity, and increasing gut permeability. This can lead to an increased risk of inflammation and immune dysregulation.
- Medication: Certain medications, particularly antibiotics, can disrupt the gut microbiome by killing off beneficial bacteria and promoting the growth of pathogenic species. While antibiotics are sometimes necessary, their overuse or misuse can have long-lasting effects on gut health.
- Environment: Factors such as hygiene, exposure to pathogens, and lifestyle can also shape the gut microbiome. For example, living in an environment with limited exposure to diverse microbial species may result in a less diverse gut microbiome, potentially increasing the risk of immune-related conditions like allergies and autoimmune diseases.
Gut Microbiome and Cognitive Health
The gut microbiome plays a crucial role in cognitive health, with growing evidence suggesting that the composition and function of the gut microbiota can directly or indirectly influence brain function and mental well-being [4]. This section explores the impact of the gut microbiome on mental health, learning and memory, neurodegenerative diseases, and neuroinflammation.
Impact on Mental Health
The gut microbiome has been linked to various mental health disorders, such as depression and anxiety, through the gut-brain axis:
Depression and Anxiety
Studies have shown that individuals with depression or anxiety often exhibit an altered gut microbiome compared to healthy individuals. Dysbiosis may contribute to these disorders by increasing inflammation, altering neurotransmitter production, and affecting the stress response. Some strains of probiotics have been shown to improve mood and anxiety symptoms in both animals and humans, suggesting a potential role for gut microbiota modulation in the management of mental health disorders.
Stress Response
The gut microbiome can influence the body’s stress response, with certain bacteria producing compounds that can modulate the release of stress hormones like cortisol. An imbalanced gut microbiome can exacerbate stress-related symptoms and contribute to the development of stress-related disorders.
Influence on Learning and Memory
Emerging research suggests that the gut microbiome may impact cognitive functions like learning and memory by affecting neuroplasticity, neurotransmitter production, and inflammation [5]. Animal studies have demonstrated that germ-free mice, which lack a gut microbiome, exhibit altered memory and cognitive performance compared to conventionally raised mice. Modulation of the gut microbiome through diet or probiotic supplementation has been shown to improve learning and memory in both animals and humans.
Links to Neurodegenerative Diseases
The gut microbiome may also play a role in the development and progression of neurodegenerative diseases, such as Alzheimer’s and Parkinson’s:
Alzheimer’s Disease
Recent studies have revealed an association between dysbiosis and Alzheimer’s disease, with alterations in the gut microbiome potentially contributing to increased inflammation and the accumulation of amyloid-beta plaques, a hallmark of the disease. Modulating the gut microbiome through diet or probiotics may hold promise for the prevention or treatment of Alzheimer’s disease.
Parkinson’s Disease
The gut microbiome has been implicated in Parkinson’s disease, with studies suggesting that changes in the gut microbiota may contribute to the aggregation of alpha-synuclein, a protein associated with the disease. Further research is needed to determine the exact mechanisms and potential therapeutic interventions targeting the gut microbiome for Parkinson’s disease.
Role in Neuroinflammation
The gut microbiome can influence neuroinflammation, which has been implicated in various neurological and psychiatric disorders. Dysbiosis can lead to increased gut permeability and the release of pro-inflammatory compounds, which can cross the blood-brain barrier and trigger inflammation in the brain. By modulating the gut microbiome and reducing inflammation, it may be possible to alleviate symptoms and slow the progression of cognitive decline associated with neuroinflammatory conditions.

Promoting a Healthy Gut Microbiome
Nurturing a healthy gut microbiome is essential for supporting the gut-brain axis and promoting optimal cognitive health. This section discusses various strategies for promoting a healthy gut microbiome, including diet and nutrition, stress management techniques, minimizing exposure to antibiotics, and the importance of a healthy lifestyle.
Diet and Nutrition
Diet plays a crucial role in shaping the gut microbiome. By making mindful dietary choices, you can encourage the growth of beneficial bacteria and support a healthy gut-brain axis:
- Prebiotics and probiotics: Incorporate prebiotic-rich foods, such as garlic, onions, asparagus, and bananas, into your diet to support the growth of beneficial bacteria. Probiotic-rich foods, like yogurt, kefir, sauerkraut, and kimchi, can introduce beneficial bacteria directly into your gut, promoting a healthy microbiome.
- Fiber-rich foods: Consume a diet rich in fiber, particularly from plant-based sources, such as fruits, vegetables, whole grains, and legumes. Fiber supports the growth of beneficial bacteria and the production of short-chain fatty acids, which have anti-inflammatory properties and promote gut health.
- Omega-3 fatty acids: Include sources of omega-3 fatty acids, such as fatty fish, walnuts, flaxseeds, and chia seeds, in your diet. Omega-3 fatty acids have been shown to reduce inflammation and support a healthy gut microbiome.
Stress Management Techniques
Managing stress is essential for maintaining a healthy gut microbiome and supporting the gut-brain axis:
- Mindfulness and meditation: Incorporate mindfulness practices, such as meditation, deep breathing exercises, and yoga, into your daily routine to help reduce stress and promote relaxation.
- Exercise: Engage in regular physical activity, which has been shown to reduce stress, improve mood, and positively impact gut health by promoting the growth of beneficial bacteria.
- Sleep hygiene: Prioritize good sleep hygiene by establishing a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment. Adequate sleep is essential for reducing stress and supporting a healthy gut microbiome.
Minimizing Exposure to Antibiotics
While antibiotics can be life-saving, their overuse or misuse can disrupt the gut microbiome and have long-lasting effects on gut health. Use antibiotics only when prescribed by a healthcare professional and follow the recommended dosage and duration to minimize the impact on your gut microbiome.
Importance of a Healthy Lifestyle
Maintaining a healthy lifestyle that includes a balanced diet, regular exercise, stress management, and adequate sleep can go a long way in supporting a healthy gut microbiome and promoting cognitive well-being. By making conscious choices to prioritize gut health, you can harness the power of the gut-brain axis and foster optimal mental and physical health.
Future Research and Clinical Implications of the Gut-Brain Axis
As our understanding of the gut-brain axis and the gut microbiome continues to expand, so does the potential for new research avenues and clinical applications in cognitive health. Here we highlight some of the key areas for future research and the potential implications for the prevention, diagnosis, and treatment of cognitive and mental health disorders.
Personalized Microbiome Interventions
One promising area of research is the development of personalized microbiome interventions tailored to an individual’s unique gut microbial profile [6]. By understanding the specific imbalances in a person’s gut microbiome, targeted interventions, such as customized probiotics or dietary recommendations, could be developed to address specific health issues related to cognitive function and mental health.
Microbiome-based Diagnostics
The gut microbiome may serve as a source of novel biomarkers for cognitive and mental health disorders. By identifying microbial signatures associated with specific conditions, researchers could potentially develop new diagnostic tools that rely on the analysis of an individual’s gut microbiome. This could lead to earlier detection and more accurate diagnosis of cognitive and mental health disorders, enabling timely and targeted interventions.
Microbiome-targeted Therapeutics
The gut microbiome holds promise as a target for the development of new therapeutics aimed at modulating brain function and treating cognitive and mental health disorders. Potential treatments could include the use of probiotics, prebiotics, or fecal microbiota transplantation (FMT) to restore a healthy gut microbiome and improve cognitive health. Additionally, harnessing the power of specific microbial metabolites, such as short-chain fatty acids or neurotransmitters, could lead to the development of novel compounds with therapeutic potential.
Integration of Gut Microbiome Research in Clinical Practice
As our understanding of the gut-brain axis and the role of the gut microbiome in cognitive health deepens, it is essential to integrate this knowledge into clinical practice. Healthcare professionals should consider the gut microbiome when assessing patients’ overall health and well-being and recommend evidence-based interventions, such as dietary modifications or probiotic supplementation, when appropriate.
Longitudinal Studies and Large-scale Clinical Trials
To fully understand the impact of the gut microbiome on cognitive health, further research is needed, including long-term, large-scale studies and clinical trials. These studies should focus on elucidating the mechanisms by which the gut microbiome influences brain function, identifying specific microbial taxa and metabolites with therapeutic potential, and determining the efficacy and safety of microbiome-targeted interventions in diverse populations.

Nutritional Supplements That Benefit the Gut-Brain Axis
Various nutritional supplements are thought to benefit the gut-brain axis by promoting a healthy gut microbiome and supporting cognitive health.
Probiotics
Probiotics are live microorganisms, often referred to as “good” or “friendly” bacteria, that provide health benefits when consumed in adequate amounts. They can be found in various fermented foods or taken as dietary supplements. Probiotics have the potential to benefit the gut-brain axis through several mechanisms:
- Modulating gut microbiome: Probiotics can help restore and maintain a healthy gut microbiome by introducing beneficial bacteria, which can outcompete harmful bacteria, enhance gut barrier function, and promote a balanced microbial ecosystem. A healthy gut microbiome is essential for optimal communication along the gut-brain axis.
- Producing neurotransmitters: Some strains of probiotics have the ability to produce neurotransmitters, such as serotonin, dopamine, and gamma-aminobutyric acid (GABA), which play a critical role in mood regulation and cognitive function. By increasing the production of these neurotransmitters in the gut, probiotics can indirectly influence brain function and mental well-being.
- Reducing inflammation: Probiotics can help modulate the immune system and reduce inflammation in the gut. Chronic inflammation can negatively impact the gut-brain axis and contribute to cognitive and mental health disorders. By lowering inflammation, probiotics may help improve cognitive function and mental health.
- Improving gut barrier function: Probiotics can help maintain the integrity of the gut barrier, preventing the leakage of harmful substances into the bloodstream, which can trigger inflammation and disrupt brain function. A healthy gut barrier is crucial for maintaining a well-functioning gut-brain axis.
- Modulating stress response: Some strains of probiotics have been shown to reduce stress-related behaviors and cortisol levels in both animal and human studies, suggesting their potential role in modulating the stress response along the gut-brain axis.
Prebiotics
Prebiotics are non-digestible dietary fibers that promote the growth and activity of beneficial bacteria in the gut. They can be found in various plant-based foods, such as garlic, onions, asparagus, bananas, and whole grains. Prebiotics can benefit the gut-brain axis through several mechanisms:
- Supporting a healthy gut microbiome: Prebiotics serve as a food source for beneficial bacteria, such as Bifidobacteria and Lactobacilli, helping them to thrive in the gut. By promoting the growth of these beneficial bacteria, prebiotics contribute to a balanced and diverse gut microbiome, which is essential for maintaining optimal communication along the gut-brain axis.
- Production of short-chain fatty acids (SCFAs): The fermentation of prebiotics by gut bacteria results in the production of SCFAs, such as butyrate, propionate, and acetate. SCFAs have numerous beneficial effects on gut health, including providing energy for colon cells, maintaining gut barrier integrity, and modulating the immune system. SCFAs can also cross the blood-brain barrier, where they may have direct effects on brain function, such as modulating inflammation and neuroplasticity.
- Reducing inflammation: Prebiotics can help modulate the immune system and reduce inflammation in the gut by promoting the growth of anti-inflammatory bacteria and increasing the production of SCFAs. Chronic inflammation can negatively impact the gut-brain axis and contribute to cognitive and mental health disorders. By lowering inflammation, prebiotics may help improve cognitive function and mental health.
- Modulating neurotransmitter production: Prebiotics can indirectly influence the production of neurotransmitters, such as serotonin, by promoting the growth of specific bacteria that have the ability to produce these signaling molecules. A balanced production of neurotransmitters is crucial for maintaining optimal brain function and mental well-being.
- Stress response and neuroprotection: Some studies have suggested that prebiotics can modulate the stress response and promote neuroprotection by increasing the production of brain-derived neurotrophic factor (BDNF), a protein that supports the survival and growth of neurons. By modulating the stress response and promoting neuroprotection, prebiotics may help improve cognitive function and mental health.
Omega-3 Fatty Acids
Omega-3 fatty acids are a type of essential polyunsaturated fatty acids that play a crucial role in various aspects of human health. They are found in foods such as fatty fish, walnuts, flaxseeds, and chia seeds. Omega-3 fatty acids, particularly eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), can benefit the gut-brain axis through several mechanisms [7]:
- Anti-inflammatory effects: Omega-3 fatty acids possess potent anti-inflammatory properties, helping to reduce inflammation in both the gut and the brain. By lowering inflammation, omega-3 fatty acids can contribute to improved gut health and support the gut-brain axis communication.
- Neuroprotection and neurogenesis: DHA, a primary component of brain cell membranes, is essential for maintaining the structural and functional integrity of neurons. Omega-3 fatty acids, particularly DHA, support neuroprotection, neurogenesis, and neuronal plasticity, which are crucial for optimal brain function and cognitive health.
- Modulation of neurotransmitter systems: Omega-3 fatty acids can influence the production, release, and function of neurotransmitters such as serotonin and dopamine, which play a critical role in mood regulation, memory, and learning. By modulating neurotransmitter systems, omega-3 fatty acids can indirectly support the gut-brain axis and promote cognitive and mental well-being.
- Support for a healthy gut microbiome: Some studies have suggested that omega-3 fatty acids can positively impact the composition and diversity of the gut microbiome. A diverse and balanced gut microbiome is essential for maintaining optimal gut-brain axis communication.
- Stress response and mood regulation: Omega-3 fatty acids have been shown to modulate the stress response, reduce symptoms of anxiety and depression, and improve overall mood. These effects can contribute to the maintenance of a healthy gut-brain axis and support mental health.
Curcumin
Curcumin, the primary bioactive compound found in the spice turmeric, has gained attention for its potential health benefits, including its effects on the gut-brain axis. Curcumin may benefit the gut-brain axis through several mechanisms [8]:
- Anti-inflammatory effects: Curcumin has potent anti-inflammatory properties and can help reduce inflammation in both the gut and the brain. By lowering inflammation, curcumin can contribute to improved gut health, support gut-brain axis communication, and promote cognitive and mental well-being.
- Antioxidant properties: Curcumin acts as a powerful antioxidant, neutralizing free radicals and reducing oxidative stress in the body. Oxidative stress has been implicated in the development of various cognitive and mental health disorders. By mitigating oxidative stress, curcumin may help support brain function and mental health.
- Neuroprotective effects: Curcumin has been shown to have neuroprotective properties, promoting neuronal survival, reducing neurodegeneration, and enhancing neuroplasticity. These effects may contribute to improved brain function, memory, and learning, supporting a healthy gut-brain axis.
- Modulation of neurotransmitter systems: Curcumin can influence the production, release, and function of neurotransmitters such as serotonin and dopamine, which play a critical role in mood regulation, memory, and learning. By modulating neurotransmitter systems, curcumin can indirectly support the gut-brain axis and promote cognitive and mental well-being.
- Support for a healthy gut microbiome: Some studies have suggested that curcumin can positively impact the composition and diversity of the gut microbiome by promoting the growth of beneficial bacteria and inhibiting the growth of harmful bacteria. A diverse and balanced gut microbiome is essential for maintaining optimal gut-brain axis communication.
- Amelioration of neuroinflammation: Curcumin has been shown to reduce neuroinflammation by inhibiting the activation of microglial cells, which are involved in the inflammatory response within the brain. By reducing neuroinflammation, curcumin may help protect brain function and support the gut-brain axis.
References
[1] Vagus Nerve
[2] Gut Microbiome Communication: The Gut-Organ Axis
[3] Gut Microbiota and Immune System Interactions
[4] Relationship between the gut microbiome and brain function
[5] The Impact of Chronic Inflammation on Brain Health and Ways to Combat It
[6] Microbiome at the Frontier of Personalized Medicine
[7] Eicosapentaenoic and docosahexaenoic acids attenuate hyperglycemia through the microbiome-gut-organs axis
[8] Exploring the Neuroprotective Mechanism of Curcumin Inhibition of Intestinal Inflammation against Parkinson’s Disease Based on the Gut-Brain Axis