Thyroid hormones play a vital and often overlooked role in maintaining optimal brain health and cognitive function. These hormones, primarily thyroxine (T4) and triiodothyronine (T3), regulate various physiological processes throughout the body. However, their impact on brain development, memory, learning, and emotional regulation is particularly significant.
Contents
About Thyroid Hormones
Thyroid hormones are essential for proper growth and development, as well as the regulation of metabolic processes in the body. They are responsible for controlling the rate at which cells use energy, impacting various aspects of health, including temperature regulation, heart function, and digestion. When it comes to the brain, these hormones are crucial for the normal development and functioning of the central nervous system. Their involvement in brain health is not only significant during the early stages of life but also throughout adulthood, as they continue to modulate cognitive processes.
Thyroid Hormone Production and Regulation
Understanding the role of thyroid hormones in brain health and cognition requires a fundamental grasp of their production and regulation. In this section, we will discuss the anatomy of the thyroid gland, the process of hormone synthesis, and the feedback mechanism responsible for maintaining hormonal balance.
Thyroid Gland Anatomy
The thyroid gland is a butterfly-shaped endocrine organ located in the neck, just below the Adam’s apple. It consists of two lobes connected by a narrow tissue bridge called the isthmus. The primary function of the thyroid gland is to produce and secrete thyroid hormones, which are vital for numerous physiological processes, including brain function.
Hormone Synthesis Process
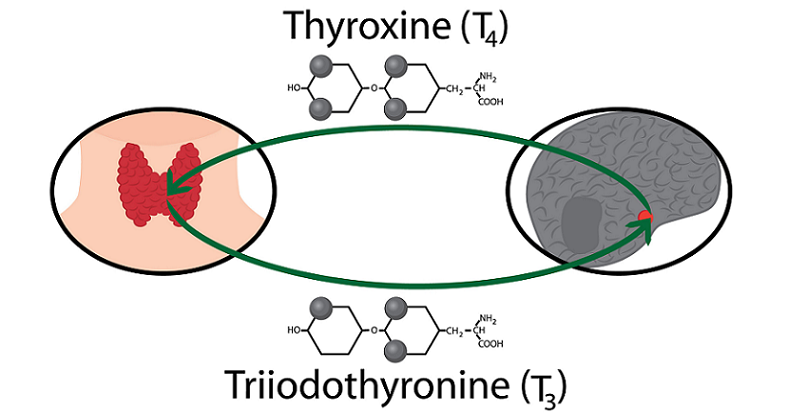
The production of thyroid hormones is a complex process involving several key components. Two primary hormones, thyroxine (T4) and triiodothyronine (T3), are synthesized and released by the thyroid gland [1].
Role of Iodine
Iodine, a trace element found in certain foods and supplements, is essential for the production of thyroid hormones. The thyroid gland actively absorbs iodine from the bloodstream and incorporates it into the hormones’ molecular structure. Inadequate iodine intake can lead to impaired thyroid hormone production, resulting in various health problems, including cognitive dysfunction.
Production of Thyroxine (T4) and Triiodothyronine (T3)
Thyroid hormone production begins with the synthesis of thyroglobulin, a protein produced by the thyroid gland’s cells. Iodine molecules are attached to thyroglobulin, forming the precursors of T4 and T3. The enzyme thyroid peroxidase (TPO) then catalyzes the conversion of these precursors into T4 and T3. The thyroid gland releases T4 and T3 into the bloodstream, where they are transported to target tissues, including the brain.
Hypothalamic-Pituitary-Thyroid Axis
The production and release of thyroid hormones are regulated by a complex feedback system involving the hypothalamus, the pituitary gland, and the thyroid gland, collectively known as the hypothalamic-pituitary-thyroid (HPT) axis [2].
Thyrotropin-Releasing Hormone (TRH)
The hypothalamus, a region in the brain responsible for controlling various hormonal systems, senses changes in blood levels of thyroid hormones. When levels are low, the hypothalamus releases thyrotropin-releasing hormone (TRH) into the bloodstream, signaling the pituitary gland to produce and secrete thyroid-stimulating hormone (TSH).
Thyroid-Stimulating Hormone (TSH)
In response to TRH, the pituitary gland releases TSH, which stimulates the thyroid gland to produce and release more T4 and T3. As blood levels of thyroid hormones rise, they inhibit the release of TRH and TSH, effectively establishing a feedback loop to maintain hormonal balance.
Feedback Mechanism
The HPT axis’s feedback mechanism helps maintain optimal levels of thyroid hormones in the body [3]. When thyroid hormone levels are too high or too low, the axis adjusts the release of TRH and TSH accordingly to normalize hormone production and maintain homeostasis. This delicate balance is crucial for optimal brain function and cognitive performance.
Thyroid Hormones and Brain Development
The impact of thyroid hormones on brain development is profound and multifaceted. These hormones play crucial roles in various stages of brain development, starting from prenatal life and continuing into adulthood. In this section, we will explore how thyroid hormones contribute to the growth and maturation of the brain throughout different life stages.
Prenatal Brain Development
During fetal development, thyroid hormones play a vital role in shaping the brain’s structure and function. They influence several critical processes, such as neuronal migration, synaptogenesis, and myelination.
Neuronal Migration
Neuronal migration is the process by which newly formed neurons move to their appropriate locations within the developing brain [4]. This movement is crucial for establishing the brain’s functional architecture. Thyroid hormones regulate the expression of genes involved in neuronal migration, ensuring that neurons reach their final destinations and form the correct neural networks.
Synaptogenesis
Synaptogenesis is the formation of synapses, the connections between neurons that enable them to communicate with each other. Thyroid hormones play a critical role in regulating synaptogenesis, promoting the growth and differentiation of neurons and the establishment of synaptic connections. Disruptions in thyroid hormone levels during prenatal development can lead to abnormal synapse formation, which may have long-lasting effects on cognitive function.
Myelination
Myelination is the process by which nerve fibers are insulated with a fatty substance called myelin, enabling rapid and efficient transmission of electrical signals between neurons [5]. Thyroid hormones are essential for myelination during fetal development, promoting the maturation of oligodendrocytes, the cells responsible for producing myelin. Insufficient thyroid hormone levels during this critical period can result in delayed or incomplete myelination, which may contribute to cognitive impairments later in life.
Postnatal Brain Development
Thyroid hormones continue to play an important role in brain development after birth. They are involved in several ongoing processes, such as neurogenesis, synaptic plasticity, and glial cell development.
Neurogenesis
Neurogenesis is the process of generating new neurons throughout an individual’s lifetime. While the majority of neurons are formed prenatally, neurogenesis continues to occur in specific regions of the adult brain, such as the hippocampus, a structure involved in learning and memory. Thyroid hormones are essential for adult neurogenesis, promoting the proliferation and differentiation of neural stem cells.
Synaptic Plasticity
Synaptic plasticity refers to the ability of synapses to change in strength and efficiency in response to new experiences, a process critical for learning and memory formation. Thyroid hormones modulate synaptic plasticity by regulating the expression of genes involved in synaptic transmission and by influencing the availability of neurotransmitters. These hormones also contribute to the maintenance of long-term potentiation, a cellular mechanism underlying memory storage.
Glial Cell Development
Glial cells are non-neuronal cells that support and protect neurons in the central nervous system [6]. They play a crucial role in maintaining the brain’s structure and function, including modulating synaptic activity, providing metabolic support to neurons, and regulating the brain’s immune response. Thyroid hormones are essential for the proper development and function of glial cells, ensuring the ongoing maintenance of a healthy brain.
Thyroid Hormones and Cognitive Function
Thyroid hormones have a significant impact on various aspects of cognitive function, including memory, learning, attention, and emotional regulation. In this section, we will explore the mechanisms by which thyroid hormones influence these cognitive processes and how disruptions in thyroid hormone levels can affect cognitive performance.
Memory and Learning
Thyroid hormones play a crucial role in memory formation and learning, particularly by modulating neurogenesis and synaptic plasticity in the hippocampus, a brain structure essential for these cognitive processes.
Hippocampal Neurogenesis
As mentioned earlier, thyroid hormones promote the proliferation and differentiation of neural stem cells in the hippocampus, contributing to the ongoing generation of new neurons. These newly formed neurons integrate into existing neural circuits, enhancing the brain’s capacity for learning and memory. Disruptions in thyroid hormone levels can impair hippocampal neurogenesis, leading to deficits in memory formation and retrieval.
Long-Term Potentiation
Long-term potentiation (LTP) is a cellular mechanism underlying memory storage, characterized by the strengthening of synaptic connections between neurons in response to repeated stimulation [7]. Thyroid hormones facilitate the induction and maintenance of LTP by modulating the expression of genes involved in synaptic transmission and by influencing the availability of neurotransmitters. Impaired thyroid hormone function can compromise LTP, resulting in diminished learning and memory capabilities.
Attention and Executive Function
Thyroid hormones also influence cognitive processes such as attention and executive function, which encompass a range of higher-order abilities, including planning, decision-making, and cognitive flexibility. These processes are primarily mediated by the prefrontal cortex, a brain region sensitive to thyroid hormone levels.
Prefrontal Cortex Function
Thyroid hormones regulate the maturation and function of the prefrontal cortex by modulating the expression of genes involved in neuronal development, synaptic plasticity, and neurotransmitter release. Optimal thyroid hormone levels are essential for maintaining the structural and functional integrity of the prefrontal cortex, thereby supporting attention and executive function.
Dopamine Regulation
Dopamine, a neurotransmitter involved in attention and executive function, is regulated by thyroid hormones. These hormones influence dopamine synthesis, release, and receptor function, thereby modulating dopaminergic neurotransmission in the prefrontal cortex. Disruptions in thyroid hormone levels can result in altered dopamine function, contributing to deficits in attention and executive function.
Mood and Emotional Regulation
Thyroid hormones also play a critical role in mood and emotional regulation, affecting the balance of neurotransmitters such as serotonin and norepinephrine and modulating the function of the limbic system, a brain network responsible for processing emotions.
Serotonin and Norepinephrine Balance
Thyroid hormones regulate the synthesis, release, and metabolism of serotonin and norepinephrine, two neurotransmitters implicated in mood regulation [8]. Imbalances in thyroid hormone levels can disrupt the normal balance of these neurotransmitters, leading to mood disturbances, such as depression or anxiety.
Limbic System Function
The limbic system, comprising brain structures such as the amygdala, hippocampus, and hypothalamus, is crucial for emotional processing and regulation. Thyroid hormones modulate the function of the limbic system by influencing the expression of genes involved in synaptic transmission and by regulating the availability of neurotransmitters. Disruptions in thyroid hormone function can lead to impaired emotional regulation, contributing to mood disorders and other psychiatric conditions.
Thyroid Hormone Imbalances and Cognitive Impairment
Disruptions in thyroid hormone levels can have significant consequences for cognitive function. In this section, we will discuss the cognitive implications of two common thyroid hormone imbalances: hypothyroidism and hyperthyroidism. We will also address the importance of accurate diagnosis and effective treatment strategies for managing the cognitive symptoms associated with these conditions.
Hypothyroidism
Hypothyroidism is a condition characterized by insufficient production or function of thyroid hormones, which can result from various causes, including iodine deficiency, autoimmune disease, and congenital defects [9]. Cognitive impairments associated with hypothyroidism include memory deficits, reduced attention and executive function, and mood disturbances.
Memory Deficits
Individuals with hypothyroidism often experience memory impairments due to disrupted hippocampal neurogenesis and compromised long-term potentiation. These disruptions can manifest as difficulty encoding new information, retrieving stored memories, and adapting to new learning tasks.
Reduced Attention and Executive Function
Hypothyroidism can also lead to deficits in attention and executive function, resulting from impaired prefrontal cortex function and altered dopamine regulation. These deficits may present as difficulty concentrating, planning, making decisions, and adapting to new situations.
Mood Disturbances
Mood disturbances, such as depression and anxiety, are common among individuals with hypothyroidism. These emotional symptoms result from imbalances in serotonin and norepinephrine levels and disrupted limbic system function.
Hyperthyroidism
Hyperthyroidism is a condition characterized by excessive production or function of thyroid hormones, which can result from various causes, including autoimmune disease, thyroid nodules, and excessive iodine intake [10]. Cognitive impairments associated with hyperthyroidism include memory deficits, reduced attention and executive function, and mood disturbances.
Memory Deficits
Like hypothyroidism, hyperthyroidism can lead to memory impairments due to disruptions in hippocampal neurogenesis and long-term potentiation. These disruptions can result in difficulty encoding and retrieving memories and adjusting to new learning tasks.
Reduced Attention and Executive Function
Hyperthyroidism can also lead to deficits in attention and executive function, resulting from overstimulation of the prefrontal cortex and altered dopamine regulation. These deficits may manifest as difficulty concentrating, impulsivity, and reduced cognitive flexibility.
Mood Disturbances
Individuals with hyperthyroidism often experience mood disturbances, such as irritability, anxiety, and emotional instability. These emotional symptoms result from imbalances in serotonin and norepinephrine levels and overactivation of the limbic system.
Diagnosis and Treatment
Accurate diagnosis and effective treatment of thyroid hormone imbalances are essential for managing the associated cognitive symptoms. Diagnostic approaches typically involve blood tests to measure thyroid hormone levels and thyroid-stimulating hormone (TSH) levels. Treatment options for hypothyroidism may include thyroid hormone replacement therapy, while hyperthyroidism treatments may involve antithyroid medications, radioactive iodine, or surgery.
Importance of Timely Diagnosis
Timely diagnosis of thyroid hormone imbalances is critical for mitigating the cognitive consequences of these conditions. Early intervention can help prevent or minimize cognitive deficits, improve mood and emotional regulation, and enhance overall quality of life.
Effective Treatment Strategies
Effective treatment strategies for thyroid hormone imbalances can significantly improve cognitive function and emotional well-being. For individuals with hypothyroidism, thyroid hormone replacement therapy can help restore optimal hormone levels, thereby alleviating cognitive and mood symptoms.
For those with hyperthyroidism, treatments that reduce thyroid hormone production or function can help normalize hormone levels and improve cognitive and emotional symptoms. In some cases, additional interventions, such as cognitive-behavioral therapy or medication for mood disorders, may be necessary to address the full spectrum of cognitive and emotional impairments associated with thyroid hormone imbalances.
Monitoring and Adjusting Treatment
Regular monitoring of thyroid hormone and TSH levels is essential to ensure the effectiveness of treatment and to make adjustments as needed. Close collaboration between healthcare providers and patients is crucial for optimizing treatment strategies and achieving the best possible outcomes in terms of cognitive function and emotional well-being.
Diagnosis and Treatment of Thyroid Dysfunction
Proper diagnosis and treatment of thyroid dysfunction are essential for managing the cognitive and emotional symptoms associated with thyroid hormone imbalances. In this section, we will discuss the diagnostic approaches and treatment options available for addressing thyroid dysfunction and ensuring optimal brain health and cognitive function.
Diagnostic Approaches
Diagnosing thyroid dysfunction involves a combination of clinical evaluation and laboratory testing. The primary diagnostic tools include blood tests that measure thyroid hormone levels and thyroid-stimulating hormone (TSH) levels.
Blood Tests
Blood tests are the primary means of diagnosing thyroid dysfunction. These tests measure the levels of thyroid hormones, specifically triiodothyronine (T3), thyroxine (T4), and thyroid-stimulating hormone (TSH) [11]. Abnormal TSH levels, in conjunction with abnormal T3 or T4 levels, can indicate either hypothyroidism or hyperthyroidism.
Imaging Studies
In some cases, imaging studies such as ultrasound, computed tomography (CT) scans, or magnetic resonance imaging (MRI) may be used to visualize the thyroid gland and detect structural abnormalities, such as nodules or inflammation, that could be contributing to thyroid dysfunction.
Additional Tests
Depending on the suspected cause of thyroid dysfunction, additional tests may be necessary. For example, tests for thyroid autoantibodies can help identify autoimmune thyroid disorders, such as Hashimoto’s thyroiditis or Graves’ disease, which are common causes of hypothyroidism and hyperthyroidism, respectively.
Treatment Options
The treatment of thyroid dysfunction depends on the underlying cause and the severity of the hormone imbalance. Common treatment options include thyroid hormone replacement therapy for hypothyroidism, antithyroid medications for hyperthyroidism, and, in some cases, surgical intervention or radioactive iodine therapy.
Thyroid Hormone Replacement Therapy
For individuals with hypothyroidism, thyroid hormone replacement therapy is the standard treatment [12]. This typically involves the administration of synthetic thyroxine (T4) or a combination of synthetic T4 and triiodothyronine (T3) to restore optimal hormone levels and alleviate cognitive and mood symptoms.
Antithyroid Medications
For those with hyperthyroidism, antithyroid medications are often prescribed to reduce thyroid hormone production or block their effects on the body. Commonly prescribed antithyroid medications include methimazole and propylthiouracil. These medications can help normalize hormone levels and improve cognitive and emotional symptoms.
Radioactive Iodine Therapy and Surgery
In some cases of hyperthyroidism, radioactive iodine therapy or surgery may be necessary to remove or destroy part of the thyroid gland. Radioactive iodine therapy involves the administration of a small dose of radioactive iodine, which is selectively taken up by the thyroid gland and destroys overactive thyroid tissue.
Surgical intervention, such as a thyroidectomy, involves the partial or complete removal of the thyroid gland. Both treatment options can effectively reduce thyroid hormone production and alleviate cognitive and emotional symptoms.
Ongoing Management and Monitoring
Ongoing management and monitoring of thyroid dysfunction are crucial for ensuring the effectiveness of treatment and making adjustments as needed. Regular blood tests to measure thyroid hormone and TSH levels are essential for tracking treatment progress and determining whether dosage adjustments are necessary.
Patient-Provider Collaboration
Close collaboration between patients and healthcare providers is vital for optimizing treatment strategies and achieving the best possible outcomes in terms of cognitive function and emotional well-being. Open communication and shared decision-making can help ensure that patients receive appropriate care tailored to their specific needs and circumstances.
Lifestyle Considerations
In addition to medical interventions, lifestyle factors can play a significant role in managing thyroid dysfunction and its associated cognitive and emotional symptoms. Adopting a balanced diet, engaging in regular exercise, practicing stress management techniques, and maintaining good sleep hygiene can support overall brain health and cognitive function.
References
[1] Thyroid Hormone Production and Function
[2] Thyrotropin-Releasing Hormone and the Thyroid Hormone Feedback Mechanism
[3] Physiology of the Hypothalamic-Pituitary-Thyroid Axis
[4] Neuronal Migration During Development of the Cerebellum
[5] Myelin Sheath: What They Are, Their Function, & Damage
[6] The Other Brain Cells: New Insights into What Glial Cells Do
[7] The Serotonin Brain Health Connection: Exploring the Happy Hormone
[8] Cognitive Function In Depth
[9] Hypothyroidism: Practice Essentials, Background, Pathophysiology
[10] Graves’ Disease: What It Is, Causes, Symptoms & Treatment
[11] Thyroid Function Tests
[12] Guidelines for the Treatment of Hypothyroidism: Prepared by the American Thyroid Association Task Force on Thyroid Hormone Replacement