Neurodegenerative disorders are an unsettling topic that touches the lives of millions, often leading to progressive loss of nerve cell function and, consequently, a range of debilitating symptoms. While conditions like Alzheimer’s and Parkinson’s Disease receive much of the spotlight, it’s crucial to turn our attention to less commonly known yet equally devastating disorders. One such condition is Neuronal Ceroid Lipofuscinosis (NCL), a rare genetic ailment that primarily affects children and leads to severe neurological impairment. The rarity of NCL often leaves it overlooked in the realm of medical research and public awareness, making it all the more essential to shed light on it.
Contents
- Introduction to Neurodegenerative Disorders and NCL
- What Is Neuronal Ceroid Lipofuscinosis (NCL)?
- The Underlying Biology of NCL
- NCL Clinical Presentation
- Treatment and Management of NCL
- Psychological and Social Implications of NCL
- References
Introduction to Neurodegenerative Disorders and NCL
Neurodegenerative disorders are conditions that involve the progressive degeneration or death of nerve cells, also known as neurons, leading to a range of symptoms affecting movement, cognition, and other functions. While the causes and manifestations can vary widely from one disorder to another, what they have in common is the irreversible damage they inflict on the nervous system over time.
Introducing Neuronal Ceroid Lipofuscinosis (NCL)
Now that we have a broader understanding of neurodegenerative diseases, let’s narrow our focus to Neuronal Ceroid Lipofuscinosis. NCL comprises a family of disorders primarily affecting children, leading to an accelerated loss of neurological functions. Symptoms often include vision loss, seizures, and motor function deterioration, among others. Its rarity often results in late diagnosis, posing additional challenges for affected families and clinicians alike.
Importance of Understanding Rare Diseases
You might wonder why there’s a need to focus on such a rare condition. While it’s true that NCL affects a relatively small population, the severity of the disease and its impact on affected families cannot be overstated. Additionally, understanding rare diseases often provides insights into more common conditions and fundamental biological processes. The lessons learned from studying NCL could very well contribute to breakthroughs in the broader field of neurodegenerative research.
What Is Neuronal Ceroid Lipofuscinosis (NCL)?
After having established the broader landscape of neurodegenerative diseases and the significance of focusing on rarer conditions like NCL, it’s time to get into the specifics of what Neuronal Ceroid Lipofuscinosis actually is.
Definition and Classification of NCL
Neuronal Ceroid Lipofuscinosis (NCL) is a collective term for a group of inherited neurodegenerative disorders characterized by the accumulation of a lipid-protein complex called lipofuscin within cells. This accumulation particularly affects neurons in the brain and other tissues, leading to their premature death and resulting in progressive neurological decline.
NCL is generally classified based on the age of onset and the specific gene mutations involved. The disease can manifest in infancy, childhood, or even adulthood, with each form exhibiting varying degrees of severity and a different range of symptoms. The different types are often named based on the age at which symptoms first appear, such as Infantile NCL, Late-Infantile NCL, Juvenile NCL, and Adult NCL [1].
Types of NCL
Understanding NCL is more complex due to its multiple types, each with unique characteristics and varying prognoses. As mentioned earlier, the types are often named based on the age of onset. Here are brief descriptions of the primary types:
- Infantile NCL (INCL): Usually begins before the age of 2 and is characterized by severe motor and cognitive decline. Life expectancy is significantly shortened.
- Late-Infantile NCL (LINCL): Symptoms generally appear between ages 2-4. Similar to INCL but with a somewhat slower rate of progression.
- Juvenile NCL (JNCL): Onset occurs typically between ages 5-10, involving vision loss as an early symptom, followed by cognitive and motor decline.
- Adult NCL: Rarer than the other forms, symptoms may not appear until the late 20s or even older. The progression is generally slower, but the condition is nonetheless debilitating.
Epidemiology: Who Gets Affected?
Having covered what NCL is and its various types, it’s crucial to consider its epidemiology. While NCL is a rare disorder, its impact is global, affecting individuals across various ethnic and geographical backgrounds. However, certain types of NCL may be more prevalent in specific populations due to genetic factors.
The disease is estimated to occur in about 1 in 100,000 live births worldwide, although the prevalence can vary depending on the type and the population studied. Despite its rarity, the disease serves as a crucial subject of study for neuroscientists and geneticists due to its severe impact on affected individuals and their families [2].
The Underlying Biology of NCL
Grasping the biological mechanics that drive this disorder is crucial for both understanding the disease and contributing to future research endeavors.
The Role of Neurons in NCL
Neurons, or nerve cells, are the building blocks of the nervous system. They are responsible for transmitting information between different parts of the body. In NCL, these neurons become the sites of lipofuscin accumulation, which eventually leads to their dysfunction and death. This neuronal degeneration results in the various neurological symptoms observed in patients, such as motor skill decline, seizures, and vision loss, among others. Understanding how neurons are affected in NCL can offer valuable insights into the broader field of neurodegenerative diseases.
Genetic Factors
Before we explore the genetic components involved in NCL, it’s essential to understand why genetics play such a pivotal role in the disorder. NCL is primarily an inherited condition, meaning that genetic mutations passed down from parents to children can cause the disease. These mutations often disrupt the normal function of certain genes responsible for cellular waste management, leading to the accumulation of harmful substances like lipofuscin.
Genes Involved
Several genes have been identified as contributors to different types of NCL. Mutations in genes such as CLN1, CLN2, CLN3, and several others are known to cause various forms of the disorder. Each gene correlates with specific types of NCL and influences the age of onset, progression rate, and symptom severity.
Inheritance Patterns
NCL is usually inherited in an autosomal recessive manner, meaning that a child must inherit two mutated copies of the gene (one from each parent) to manifest the disease. However, some rarer forms of NCL follow different inheritance patterns. Knowing one’s family genetic history can be instrumental in early diagnosis and management.
Cellular Mechanisms
Now that we have a clearer understanding of the genetic basis of NCL, it’s time to look at how these genetic mutations translate into cellular dysfunction.
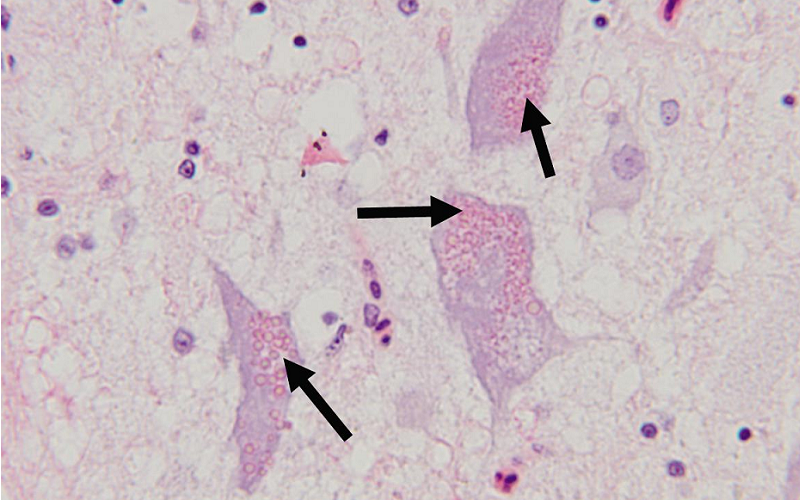
Lipofuscin Accumulation
Lipofuscin is a byproduct of cellular metabolism and is generally harmless in small amounts. However, in NCL, defective genes lead to an abnormal buildup of lipofuscin within cells, particularly neurons. This buildup interferes with normal cellular functions and eventually leads to cell death [3].
Apoptosis and Cell Death
One of the tragic realities of NCL is the premature death of neurons through a process called apoptosis, also known as programmed cell death. In NCL, the overwhelming accumulation of lipofuscin triggers this self-destruct mechanism prematurely, accelerating the degeneration of the nervous system and resulting in the varied neurological symptoms observed in NCL patients.
NCL Clinical Presentation
While understanding the underlying biology of Neuronal Ceroid Lipofuscinosis (NCL) provides an essential scientific context, it’s equally crucial to know how the disease manifests clinically. Clinical symptoms often serve as the initial indicators that prompt further investigation and diagnosis.
Common Symptoms
The first and often most noticeable aspect of NCL is the range of symptoms it presents. While these symptoms can vary significantly depending on the specific type of NCL and the age of onset, some common manifestations cut across various forms of the disorder.
Neurological Symptoms
The neurological impact of NCL is perhaps its most defining feature. Common neurological symptoms include seizures, motor function deterioration, and cognitive decline. These symptoms can profoundly affect the quality of life for those suffering from NCL and often serve as early indicators for diagnosis.
Vision Loss
Another frequent symptom is progressive vision loss. This occurs particularly in forms like Juvenile NCL and can sometimes be the initial symptom that triggers concern. Vision impairment in NCL is due to retinal degradation, another tragic manifestation of neuron death.
Behavioral Changes
In addition to physical symptoms, NCL often brings about behavioral changes. Affected children may display mood swings, irritability, and depression. Understanding these behavioral symptoms is essential for providing comprehensive care and support for affected individuals and their families.
Diagnostic Procedures
Understanding the symptoms of NCL is the first step in its diagnosis. However, for a conclusive diagnosis, several diagnostic procedures are typically employed [4].
Genetic Testing
Since NCL is primarily a genetic disorder, genetic testing is often the most definitive way to confirm a diagnosis. This involves identifying the specific mutations associated with different types of NCL.
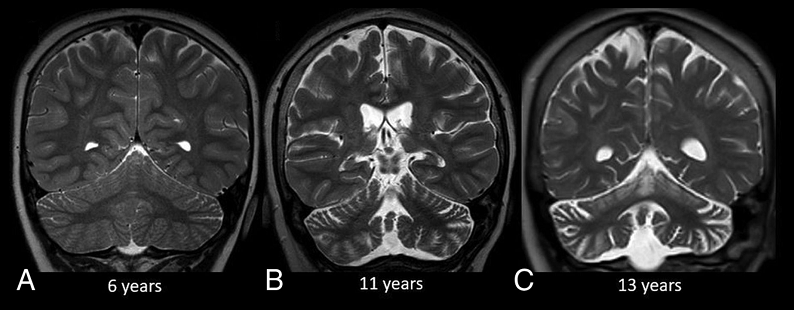
Neuroimaging
Brain scans such as MRI and CT scans can also provide valuable insights into the state of neuronal health and can help clinicians assess the degree of neurodegeneration, although these methods are generally not sufficient for a diagnosis on their own.
Enzyme Assays
For some types of NCL, the activity levels of specific enzymes may be tested. Reduced enzyme activity could serve as an indicator of the disease, complementing other diagnostic methods.
Disease Progression
Once NCL is diagnosed, families often have questions about what to expect in terms of disease progression.
Rate of Progression
The progression of NCL can vary widely depending on the type of NCL and the specific genetic mutations involved. Some forms of the disease progress rapidly, leading to severe disability within a few years, while others might have a more protracted course.
Life Expectancy
It’s a grim topic, but understanding life expectancy is crucial for families affected by NCL. Many forms of the disease, particularly those with earlier onset, significantly reduce life expectancy. This is why early diagnosis and management are so vital.
Treatment and Management of NCL
While NCL is currently incurable, a range of treatment and management options exist to help improve the quality of life for patients and their families. This section will discuss these options, from symptom-specific treatments to palliative care approaches, and even emerging therapies that show promise.
Symptom-Specific Treatments
While the underlying cause of NCL is still beyond the reach of current treatments, focusing on specific symptoms can provide some relief and improve the quality of life for those affected.
Seizure Control
Epileptic seizures are a common symptom across different types of NCL. Antiepileptic drugs (AEDs) are frequently used to manage and control these seizures, although their effectiveness can vary between individuals [5].
Motor Function Aid
As the disease progresses, motor function often deteriorates. Physical therapy and the use of mobility aids like wheelchairs can help patients maintain some degree of independence and activity for as long as possible.
Vision Support
For those experiencing vision loss, low-vision aids and occupational therapy can sometimes make daily tasks more manageable. However, it’s important to note that these measures cannot halt the progression of vision loss.
Palliative Care
Palliative care is an essential aspect of managing NCL, particularly as the disease reaches its more advanced stages.
Pain Management
Chronic pain can be a significant concern for NCL patients. Medications, along with techniques such as nerve blocks, can be employed to manage pain effectively.
Emotional and Psychological Support
Behavioral changes and psychological symptoms like depression and anxiety are common in NCL patients. Counseling, psychotherapy, and sometimes medications like antidepressants can offer relief.
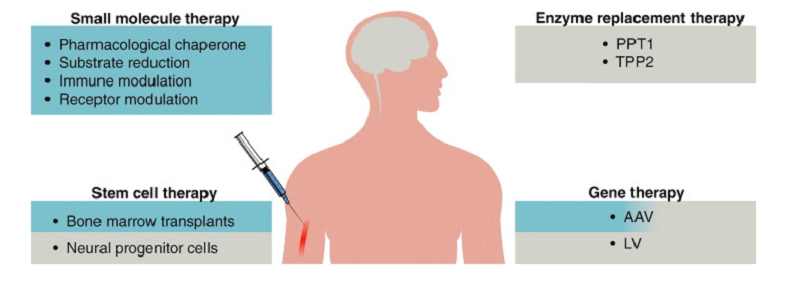
Emerging Therapies
The field of NCL research is continually evolving, and new therapies are under investigation.
Gene Therapy
Given the genetic nature of NCL, gene therapy is an area of intense research focus. While still in experimental stages, it holds the promise of treating the disease at its root cause by fixing the mutated genes.
Enzyme Replacement
For some types of NCL where enzyme deficiency is a factor, enzyme replacement therapy is being studied as a potential treatment method.
Psychological and Social Implications of NCL
While the physical and neurological symptoms of NCL are often the focus of medical discussions, the emotional and social toll on both patients and families should not be overlooked.
Emotional Impact on Patients
The emotional impact of living with NCL can be substantial and varies with the age of onset and progression of the disease.
Emotional Toll in Children
For children diagnosed with NCL, the emotional toll is often perplexing and distressing. Kids may not fully understand the disease but can sense the gravity of their condition. This can lead to feelings of fear, isolation, and depression.
Emotional Toll in Adults
For adults diagnosed with late-onset NCL, the emotional toll often involves a complex mix of anxiety, depression, and existential questions about the future, particularly in terms of independence and life goals.
Emotional Impact on Families
Just as patients experience a range of emotions, the families of those diagnosed with NCL undergo their own emotional journeys.
Coping with the Diagnosis
An NCL diagnosis can be devastating for parents and siblings, leading to a variety of emotional reactions including denial, anger, and guilt. The lifelong nature of the disease adds a level of chronic emotional stress that families must learn to manage.
Grieving and Emotional Support
The progression of NCL often involves a form of continuous grieving as symptoms worsen. Emotional support, counseling, and therapy can often help families cope with this ongoing emotional struggle.
Social Consequences
Beyond the emotional impact, the social implications of NCL are another critical aspect to consider.
Social Isolation
The visible symptoms and the challenges of disease management can sometimes lead to social isolation for both patients and families. Peer interaction and social activities become complicated, often requiring adjustments in expectations and routines.
Stigma and Misunderstanding
Due to the rarity and misunderstood nature of NCL, some families report facing social stigma and misunderstanding from their communities. Public awareness and education are crucial to combating this issue.
Supportive Measures
Dealing with the psychosocial aspects of NCL requires a multifaceted approach.
Peer Support Groups
One valuable resource is peer support groups, where families and patients can share experiences, advice, and emotional support.
Psychological Counseling
Professional psychological counseling tailored to chronic illness can provide coping strategies for both patients and families.
Educational Programs
Educational programs aimed at schools and communities can help demystify NCL and reduce the social stigma associated with the disorder.
References
[1] Neuronal Ceroid Lipofuscinoses (NCL)
[2] Neuronal Ceroid Lipofuscinoses
[3] Neuronal ceroid lipofuscinosis
[4] Adult Neuronal Ceroid Lipofuscinosis
[5] Moving towards effective therapeutic strategies for Neuronal Ceroid Lipofuscinosis