Clinical work asks for precision, kindness, and speed, often all at once. When notes pile up and alarms chirp, attention frays and empathy feels expensive. Burnout is not a personal failure. It is a predictable outcome when cognitive load stays high and recovery stays low. Here we provide a respectful fix: small measurements that flag risk early, quick resets that fit real clinics, team norms that reduce switching costs, and gentle biofeedback for steady nerves. The goal is not perfection. The goal is a shift that ends with something left in the tank for family, friends, and the next day’s patients.
Contents
- Why Burnout Emerges In Clinical Settings
- Measure What Matters: Light Metrics You Can Keep
- Between-Encounter Reset: A Two Minute Protocol You Will Actually Use
- Design The Day: Team Norms That Reduce Cognitive Load
- Recovery Outside The Shift: Protect Sleep, Energy, and Meaning
- Four Week Rollout: Make It Real Without Adding Burden
Why Burnout Emerges In Clinical Settings
Burnout is a mismatch between demands and supports. In healthcare it shows up as emotional exhaustion, lower sense of accomplishment, and a colder bedside manner than you like. Inputs are obvious: heavy caseloads, complex documentation, inbox messages that never sleep, and the emotional labor of absorbing fear and grief. Less obvious are the micro forces. Constant context switching raises cognitive costs. A narrow visual field and clenched jaw signal urgency all day, which nudges the brain toward scanning rather than listening. Sleep debt dulls working memory. Even posture can tilt decision quality, hunched shoulders pair with rushed choices far more than we admit.
Signals arrive before collapse. You notice rereads of the same line in a chart, slower retrieval of guidelines, a spike in small mistakes like wrong box clicks, and rising irritability with delays. Physiologically, resting heart rate runs a bit high, breathing gets shallow, and movement patterns grow jittery. Ignoring these signals is easy for a week and costly for a month. The antidote is a system that notices early, then responds with tiny, reliable actions that fit the day’s flow.
Compassion fatigue deserves mention. Bringing care to every room is beautiful and heavy. Rotating through grief without recovery convinces the nervous system that danger is constant. A brief reset, even two minutes, teaches your body that it can switch out of emergency mode. Rehearsed often, this switch becomes available at the exact moment you need it, right before the next conversation.
Measure What Matters: Light Metrics You Can Keep
Data should guide, not judge. Choose a tiny set of signals that you can capture without extra clicks. The point is to spot drift early, then nudge the system back toward steady. Think weather report, not performance review.
Personal signals
- Clarity rating: one to ten after a morning huddle and again after lunch. Falling scores invite a reset or a workload tweak that day.
- Time to return: seconds from finishing a reset to the first productive action, like the first meaningful sentence of a note. If the number creeps up, shorten tasks or add a microbreak.
- Fidget index: count of brief movement spikes during charting blocks. Rising fidgets predict errors and slower thinking.
Physiology, used gently
- HRV trend: a two to five minute breathing session at lunch, in for four counts and out for six, with a quick look at the short term heart rate variability trend afterward. Treat any change as a clue, not a score.
- Sleep anchors: steady wake time and a wind down checklist. Track completion, not perfection.
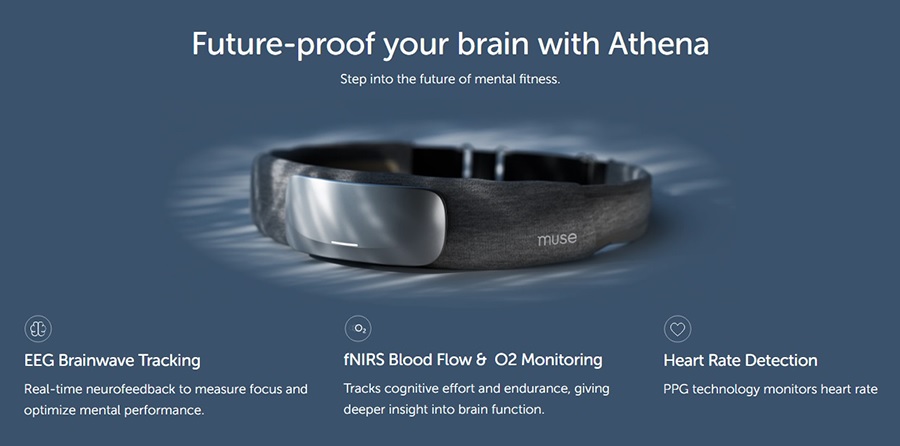
- EEG cue: some clinicians like a one minute attention settle before a tough clinic. A consumer headband, such as the Muse device, provides gentle audio cues. It is not a medical device and does not diagnose conditions. Use it as a start line, then remove it and work in silence.
Team and system signals
- Inbox load: messages per hour with two planned processing windows. If messages bleed outside windows daily, adjust staffing or templates.
- After hours charting: minutes spent documenting outside shift. A rising number is a loud signal to protect templates, dictation tools, and batch work norms.
- Interruption rate: unplanned knocks or calls per hour. Use a visible whiteboard or status light to mark do not disturb spans for complex tasks.
Privacy and boundaries matter. Keep personal metrics private unless you choose to share. Team metrics should target processes, not people. The enemy is friction and overload, not the clinician across the hall.
Between-Encounter Reset: A Two Minute Protocol You Will Actually Use
Resets work when they are short and portable. This one fits in a hallway, a stairwell, or beside a workstation. The entire sequence takes about two minutes. Run it after a heavy visit, before a family discussion, or whenever your shoulders live near your ears.
- Plant and posture, 15 seconds: stand tall with feet grounded. Unclench your jaw and let your shoulders drop. Tall posture widens the visual field and lowers the sense of threat.
- Gaze reset, 20 seconds: look 20 feet away, include the edges of your vision. Tunnel vision invites rushed decisions. A wider frame supports listening.
- Breath pacing, 60 seconds: breathe quietly in for four counts and out for six. Keep breaths small and comfortable. If edgy, make breaths even smaller but keep the rhythm.
- Label and cue, 15 seconds: use a short phrase, present and kind, or steady and clear. Repeat once. Simple cues beat complex intention statements when the pager is buzzing.
- Start line, 10 seconds: if you enjoy structure, a one minute attention settle earlier in the day with a headband such as Muse can teach the feel of steadiness. In the moment, you can recall that feel without devices.
Pair the reset with tiny environmental fixes. Face soft front light when possible, a bright screen with a bright room prevents squint and forehead tension. Keep a water bottle within reach. Place a small card near your workstation with the words plant, gaze, breathe, cue. The card is not decoration, it is a permission slip to reset before the next room.
Design The Day: Team Norms That Reduce Cognitive Load
Individual skills help, system design keeps them alive. A few agreements transform chaotic days into manageable lanes. None require new buildings. They require consistency and a shared story about attention being a scarce resource.
Flow and batching
- Charting lanes: block two or three short windows for documentation during clinic. Close the door or use a status signal. Multitask less, finish notes more.
- Inbox windows: process messages in two bursts. Outside those times, the inbox stays closed. One priority channel remains for true emergencies.
- Pre-visit templates: standardize checklists for common conditions. Templates do not replace thinking, they reduce friction.
Communication and interruptions
- Huddles: five minute morning huddle with two questions, where are the bottlenecks and what needs quiet time. Name one protected block per clinician.
- Escalation clarity: define what merits an immediate knock and what waits for a window. This lowers decision fatigue for staff who want to help but lack guidance.
- Signage and signals: a small light or card that says with patient or charting. It sets expectations without scolding.
Documentation tools
- Smart phrases and dictation: maintain a shared library that is reviewed quarterly. Remove dead phrases and add items clinicians actually use.
- After visit summary rhythm: complete the summary before the patient leaves when possible. A clear handoff reduces follow up messages later.
- Double check traps: make it easy to verify the five clicks that most often cause errors. Checklists save embarrassment and time.
Leadership sets tone. When leaders model protected lanes and humane inbox norms, staff follow. When leaders celebrate attention friendly wins, like a clinic that cut after hours charting in half, the message lands: steady clinicians help patients more.
Recovery Outside The Shift: Protect Sleep, Energy, and Meaning
Even strong clinic design cannot carry a tired brain forever. Recovery is the bridge between good days. Protect three anchors: sleep, movement, and a short ritual that drops the work story when you leave the building.
Sleep and evening routine
- Consistent wake time: your clock loves rhythm. Keep wake time steady across the week as much as schedules allow.
- Wind down, 15 minutes: dim light, two to five minutes of slow breathing, a short body scan, and two written lines for tomorrow. Keep the sequence identical on work nights.
- Screen rules: warm lighting and low brightness in the last hour. If late charting is unavoidable, end with a brief off-ramp so sleep is not a sudden cliff.
Movement and fuel
- Short sessions win: ten minute walks or mobility sets near daylight. Movement lowers static and protects mood without needing a marathon plan.
- Steady meals: anchor lunch and an afternoon snack with protein and fiber. Guard against the 4 p.m. crash that turns into late caffeine and later sleep.
Meaning and boundaries
- Transition ritual: a simple phrase at the door, work stays here, plus three slow breaths. On the commute, pick calm audio or silence rather than breaking news.
- Small wins journal: one line per evening about a moment of care that mattered. This protects the sense of impact that workload tries to steal.
- Peer connection: a ten minute check in with a colleague once a week, not to trade war stories, to trade solutions and support.
Tech can help without taking over. HRV paced breathing is a friendly nightly primer. If you enjoy biofeedback, a one minute attention settle with a headband such as Muse before wind down can mark the shift from pager to pillow. Research tools like fNIRS belong in labs, not bedrooms. Keep home tools gentle and practical.
Four Week Rollout: Make It Real Without Adding Burden
Change sticks when it is small, visible, and owned by the people doing the work. This rollout keeps the lifts light. Adjust to your specialty and clinic size.
Week 1, install the basics
- Pick two personal metrics, clarity rating and after hours charting minutes. Track quietly for yourself.
- Adopt the two minute reset. Place a small cue card at your workstation.
- Run a five minute team huddle to agree on one inbox window and one protected charting lane.
Week 2, protect attention
- Enforce inbox windows. Create a visible status signal for deep tasks.
- Add a daily ten minute walk or mobility set before dinner. Start a simple wind down.
- If you enjoy devices, test a one minute EEG settle before clinic on two days. Remove devices during patient care.
Week 3, tune workflows
- Update three templates you touch most. Retire one that wastes time.
- Measure interruption rate for a single afternoon and decide what truly merits a knock.
- Share a small win at huddle, for example, five fewer after hours messages after moving summaries earlier.
Week 4, sustain and simplify
- Keep only the metrics you use. Many clinicians retain clarity rating and after hours minutes and drop the rest.
- Write a short clinic charter that names your norms, inbox windows, charting lanes, and do not disturb signals.
- Plan a small celebration. Positive endings teach the nervous system to return to the new pattern.
If distress is high, if sleep stays broken, or if mood sinks, involve your health team. Burnout prevention is compatible with therapy, peer support, and medical care. Home routines protect function. Healthcare supports health.