The complex ecosystem of microorganisms residing within our bodies, known as the microbiome, has long been considered crucial for digestive health. But recent revelations go beyond digestion, hinting at its profound influence on our cognitive faculties. Imagine your gut’s bacterial residents playing a role in determining how well you remember or concentrate. Here we examine the intricate dance between our microbiomes and brain functions, shedding light on how imbalances in our microbial communities might impact our memory and focus.
Contents
- Understanding the Human Microbiome
- Mechanisms of Microbiome Impact on Cognitive Health
- Studies Highlighting Microbiome and Memory and Concentration Concerns
- Managing and Restoring a Healthy Microbiome
- References
Understanding the Human Microbiome
In the vast expanse of our bodies lies a universe teeming with microbial life. This microscopic community, collectively termed the microbiome, has been under intense scrutiny in recent years. The reason? Its profound influence on our health and well-being. Before we examine its ties to cognitive functions, let’s first establish a foundational understanding of the human microbiome.
Distribution Across the Body
Every corner of our body, from the skin that shields us from the environment to the depths of our digestive tract, houses a unique microbial community. These organisms are not mere squatters; they’ve evolved with us and play essential roles in our health.
Gut Microbiota
The gut, particularly the large intestine, is a hotbed for microbial activity. With trillions of microorganisms from thousands of species, it’s the most densely populated area of our microbiome. These microbes aid in digestion, produce vitamins like K and B12, and influence our immune system. Additionally, they’re involved in metabolizing dietary compounds and drugs, which can have downstream effects on our overall health.
Skin, Oral, and Other Microbiomes
While the gut garners much attention, other sites of our body have their microbial populations, each with unique roles. The skin, our largest organ, harbors a microbiome that protects against pathogens and modulates skin health. Our mouth, too, is a microbial hub, affecting not just oral health but potentially heart health and other systemic conditions. Other areas like the nasal passages, lungs, and urogenital tract have their distinct microbiomes that maintain a delicate balance to ensure optimal function.
Role in Digestion, Immunity, and More
Our symbiotic relationship with these microbes goes beyond what meets the eye. They’re not just passive inhabitants; they’re active participants in our well-being [1].
Digestion and Nutrient Synthesis
The gut microbiota plays an indispensable role in breaking down complex carbohydrates, which we cannot digest on our own. They ferment these fibers, producing short-chain fatty acids like butyrate, propionate, and acetate, which have numerous health benefits, including providing an energy source for our colon cells.
Furthermore, our microbial friends synthesize essential vitamins, as previously mentioned. These vitamins, such as B12, biotin, and folic acid, are crucial for various bodily functions, from red blood cell formation to proper nerve function.
Immune Modulation and Protection
Remarkably, a significant portion of our immune system is located in the gut, and this isn’t coincidental. The microbiome trains and modulates our immune responses. By interacting with immune cells, gut microbes help in distinguishing friend from foe, ensuring that harmful pathogens are tackled while beneficial ones or harmless substances are tolerated.
Moreover, by merely occupying the niches within our gut, these microorganisms prevent potential pathogens from gaining a foothold, offering a kind of “colonization resistance.”
Mechanisms of Microbiome Impact on Cognitive Health
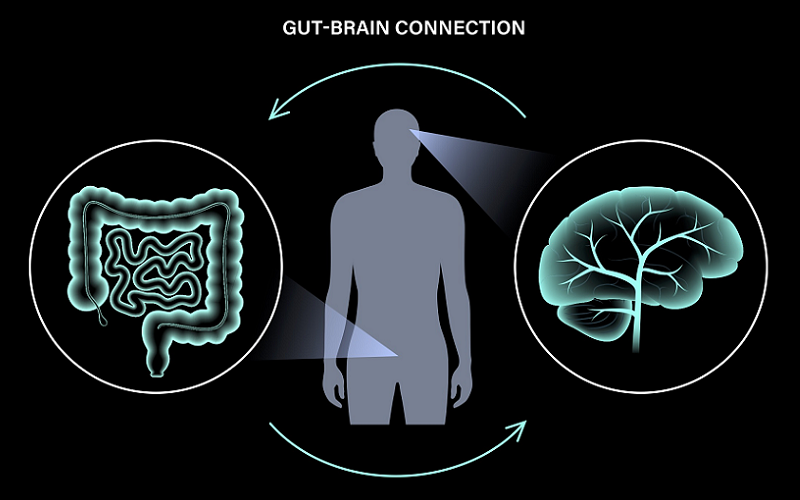
As we delve deeper into the realm of the microbiome, a compelling narrative unfolds—one that intricately ties the microscopic denizens of our gut to the vast intricacies of our brain. It’s a connection that may seem improbable at first glance. How can bacteria in our intestines affect processes as complex as memory and concentration? Yet, recent scientific insights have begun to untangle this intricate web, revealing mechanisms that underscore the profound influence of the microbiome on cognitive health.
Neurotransmitter Production
Neurotransmitters are the brain’s chemical messengers. These molecules play pivotal roles in regulating mood, sleep, appetite, and, of course, cognitive functions like memory and concentration.
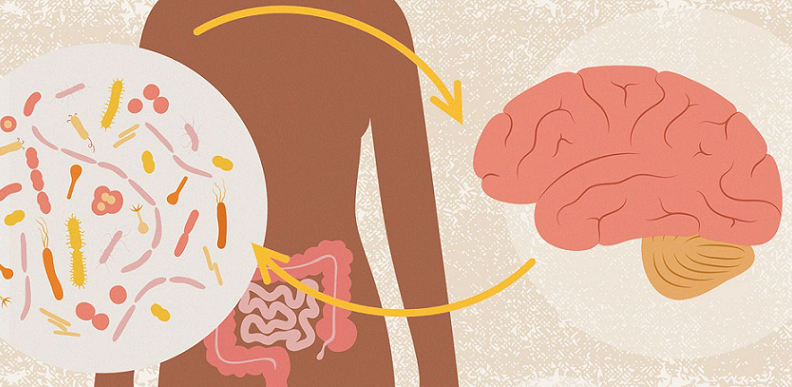
Serotonin and the Gut-Brain Connection
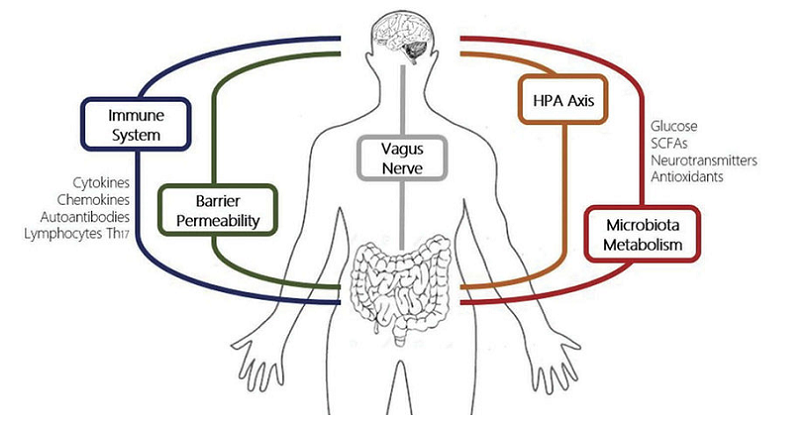
One might be surprised to learn that about 90% of the body’s serotonin—a neurotransmitter often associated with mood and well-being—is produced in the gut. Gut bacteria, through their metabolic activities, influence the production of this vital neurotransmitter. Disturbances in the microbiome, therefore, might lead to fluctuations in serotonin levels, potentially affecting mood, sleep, and cognitive processes [2].
Other Neurochemicals and Their Origins
Serotonin isn’t the only game in town. The microbiome also impacts other neurotransmitters like dopamine and gamma-aminobutyric acid (GABA). Additionally, some gut bacteria produce neuroactive compounds directly, further influencing brain function. As research continues, it’s likely that more connections between specific microbes and neurotransmitter activity will come to light.
Inflammation and Immune Responses
Inflammation, while crucial for tackling acute infections, can become problematic when chronic. There’s a growing consensus in the scientific community that chronic inflammation is a potential adversary for cognitive health.
How Inflammation Affects the Brain
Chronic inflammation has been associated with various cognitive disorders, from depression to more severe conditions like Alzheimer’s disease. The gut microbiome, when imbalanced, can produce inflammatory compounds or induce an inflammatory response in the body. This inflammation can then affect the brain either directly, by crossing the blood-brain barrier, or indirectly, by influencing various physiological pathways.
The Gut-Brain Axis and Immune System Interactions
The gut-brain axis is a bidirectional communication network between the gut and the brain. Through this axis, the immune system can relay signals from the gut microbiome to the brain and vice versa. Dysregulation in this communication, due to microbiome imbalances, might play a role in cognitive decline and other mental health conditions.
Nutrient Absorption and Brain Health
Our brain, despite being only about 2% of our body weight, consumes roughly 20% of our energy. This disproportionate energy demand means the brain is highly sensitive to nutrient availability.
Essential Nutrients for Brain Function
Several nutrients, from glucose and fatty acids to specific vitamins and minerals, are pivotal for optimal brain function. For instance, omega-3 fatty acids are crucial for neural plasticity, while B-vitamins play a role in neurotransmitter synthesis. An imbalanced gut microbiome can disrupt the absorption and metabolism of these essential nutrients [3].
How the Gut Microbiota Can Influence Nutrient Uptake
The gut microbiota aids in the breakdown and absorption of several vital nutrients. For example, certain bacteria help in fermenting dietary fibers to produce brain-beneficial compounds like butyrate. An imbalance in these microbial populations might hinder the availability of these nutrients to the brain, thereby potentially impacting cognitive functions.
Studies Highlighting Microbiome and Memory and Concentration Concerns
The hypothesis that our gut’s microbial world may influence brain functions like memory and concentration is not based on mere speculation. Scientific inquiry, in recent years, has presented a suite of evidence, drawing parallels between microbiome health and cognitive function.
Key Research Findings
Scientific studies, both on animals and humans, have started to piece together the puzzle of how our internal microbial environment relates to cognitive health. Let’s delve into some of these pivotal findings.
Animal Studies and Their Implications
Rodent studies have been foundational in this arena. One notable experiment involved transplanting the microbiota of depressed mice into germ-free mice (those without a microbiome). The previously healthy mice showcased depressive-like behaviors post-transplant, underscoring the microbiome’s influence on the brain.
In the realm of memory, research on mice has shown that a diet high in fat can alter the gut microbiota, leading to cognitive deficits. Another study found that probiotics could improve memory deficits in mice, further underscoring the microbiome’s role in cognition [4].
Human-Based Research and Observations
While animal models offer invaluable insights, human-based studies provide more direct relevance. Research on older adults has highlighted that those with diverse gut microbiota tend to perform better on cognitive tests. Another study revealed that individuals with chronic fatigue syndrome had different gut bacterial compositions compared to healthy counterparts, alongside cognitive impairments.
Furthermore, a groundbreaking study assessed the microbiota of Alzheimer’s patients, finding distinct microbial differences compared to healthy subjects. Such research nuances the possibility that microbiome imbalances could either contribute to or result from cognitive disorders.
Potential Limitations of Current Studies
As exciting as these findings are, science demands a critical lens, especially when a field is still unfolding.
Varied Factors in Human Microbiome Studies
Human microbiome research is inherently complex. Factors like diet, medication, age, genetics, and lifestyle can all impact our microbiome, making it challenging to isolate effects. Furthermore, while correlations have been observed, causality remains elusive in many cases. It’s crucial to understand that associations between the microbiome and cognitive function don’t necessarily mean one directly causes the other.
Need for Longitudinal and Comprehensive Research
Many studies to date have been cross-sectional, offering snapshots rather than comprehensive narratives. Longitudinal studies, which track changes over time, are needed to better understand the microbiome’s long-term effects on cognitive health. Additionally, multi-dimensional approaches, integrating genomics, metabolomics, and other fields, will provide a more holistic understanding.
Managing and Restoring a Healthy Microbiome
Given the mounting evidence of the microbiome’s influence on cognitive health, a question naturally emerges: how do we ensure our microbial community thrives? By proactively nurturing our microbiome, we may potentially fortify our cognitive faculties and ward off memory and concentration concerns.
Dietary Interventions
What we eat doesn’t just nourish us; it also feeds the vast army of microbes residing in our gut. Hence, diet plays a pivotal role in shaping the microbiome’s composition and functionality [5].
Prebiotics and Dietary Fibers
Prebiotics are non-digestible compounds that feed our beneficial gut bacteria. High-fiber foods, like whole grains, legumes, fruits, and vegetables, are rich in prebiotics. Regularly consuming these can encourage the growth of beneficial microbes and enhance the production of health-promoting compounds like short-chain fatty acids.
Probiotics and Fermented Foods
Probiotics are live bacteria that confer health benefits when consumed in adequate amounts. Foods like yogurt, kefir, sauerkraut, kimchi, and miso are rich in these beneficial microbes. Including them in our diet can potentially introduce and augment the abundance of health-promoting bacterial strains in our gut.
Diverse Diets for a Diverse Microbiome
Variety is not just the spice of life; it’s also the key to a thriving microbiome. A diverse diet, rich in different foods, can foster microbial diversity, which has been associated with better health outcomes, including cognitive health.
Lifestyle Factors and Practices
Beyond diet, various lifestyle practices and factors can significantly influence our microbiome.
Physical Activity
Regular exercise has been shown to positively impact gut microbiota, enhancing diversity and encouraging the growth of beneficial strains. The exact mechanisms remain under study, but the benefits of physical activity extend well beyond muscles and cardiovascular health, reaching the depths of our microbial world.
Stress Management
Chronic stress can wreak havoc on our gut microbiome, leading to imbalances that might affect cognitive health. Practices like meditation, deep breathing exercises, and ensuring adequate sleep can help manage stress and its impact on our microbial residents.
Avoiding Overuse of Antibiotics
While antibiotics are crucial in battling bacterial infections, their overuse or misuse can severely disrupt the gut microbiome. It’s essential to use these medications judiciously and under a healthcare professional’s guidance, ensuring that our microbial balance remains as undisturbed as possible.
Therapeutic Interventions
For those with significant microbiome imbalances, more targeted interventions might be necessary.
Fecal Microbiota Transplant (FMT)
While it might sound unconventional, transferring fecal matter from a healthy donor to an individual with a disrupted microbiome has shown promise in treating certain conditions. FMT aims to restore microbial balance, and while its implications for cognitive health are still under study, its potential in microbiome restoration is undeniable.
Tailored Probiotic Supplementation
Not all probiotics are created equal. Depending on an individual’s unique microbiome composition and health needs, specific probiotic strains might be more beneficial than others. Working with a healthcare professional to determine the right probiotic supplement can be an effective strategy for some individuals.
References
[1] Guts Imbalance Imbalances the Brain
[2] Microbiome and Cognitive Impairment: Can Any Diets Influence Learning Processes in a Positive Way?
[3] Microbiota and stress: a loop that impacts memory
[4] The progress of gut microbiome research related to brain disorders
[5] Does the gut play a role in dementia? Here is the evidence